The United States agency of the Department of Health and Human Services, The Food and Drug Administration FDA on Friday approved a treatment for the sickle cell disease.
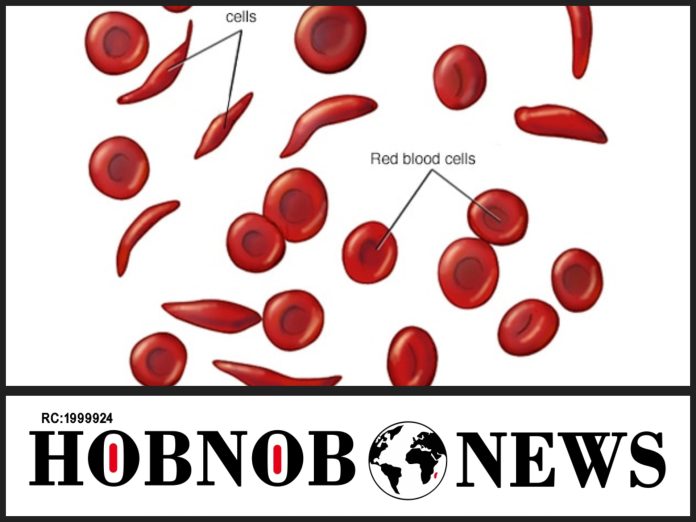
The sickle cell anaemia, a group of disorders that cause red blood cells to become misshapen and break down is a devastating illness that by 2015, have affected about 4.4 million people with an additional 43 million having the sickle cell trait.
The new therapy, dubbed as Casgevy, from Vertex Pharmaceuticals and CRISPR Therapeutics, is the first of its kind to be approved in the United States that uses the gene-editing tool CRISPR.
The CRISPR had in 2020 won the Nobel Prize in chemistry.
Dr. Alexis Thompson, chief of the division of hematology at Children’s Hospital of Philadelphia, who has previously consulted for Vertex while speaking on the gene editing tool said:
“I think this is a pivotal moment in the field. It’s been really remarkable how quickly we went from the actual discovery of CRISPR, the awarding of a Nobel Prize, and now actually seeing it being an approved product.”
In a related development, the FDA also on Friday approved Lyfgenia, a gene therapy from drugmaker Bluebird Bio, a second treatment for sickle cell disease.
The CRISPR and Lyfgenia work with the genetic modification of a patient’s own stem cells.
The only known cure for the sickle cell disease was a bone marrow transplant from a donor, but it has a limitation of having the likelihood of rejection by the immune system, and also the difficult process of finding a matching donor.
But Casgevy, approved for people ages 12 and older, do not need a donor.
With the CRISPR process, the DNA found in a patient’s stem cells is edited to remove the gene that causes the disease.
“The patient is their own donor,” Thompson said.
Dr. Asmaa Ferdjallah, a pediatric hematologist and bone marrow transplant physician at the Mayo Clinic in Rochester, Minnesota says It’s a game-changer.
“To really reimagine and re-discuss sickle cell disease as a curable disease and not as this painful and debilitating chronic disease is hope enough with this news”, he said.
Vertex however noted that the new therapy will cost a fortune, with a $2.2 million cost per patient, excluding the cost of care associated with the treatment, like a stay in the hospital or chemotherapy.
“We really have to make sure that it is accessible,” said Dr. Rabi Hanna, a pediatric hematologist-oncologist at the Cleveland Clinic who has previously served on the advisory board for Vertex.
“This could be an equalizer for people with sickle cell because many patients cannot pursue career options” because of the illness.
“It’s something families have been aware of in the early research stage, and they’ve been very patiently waiting for years,” Ferdjallah said. “It’s been eagerly awaited by patients and families, but also by providers and physicians.”
The FDA in its approval added a caveat; noting that Lyfgenia in rare cases the treatment can cause certain blood cancers.
A director of the Office of Therapeutic Products in the FDA’s Center for Biologics Evaluation and Research, Dr. Nicole Verdun, said Lyfgenia was given the warning after two patients who got the therapy in a clinical trial died from a form of leukemia.
Even though it is not clear if the gene therapy itself or another part of the treatment process, caused the cancer, but Verdun said the agency thought the deaths “rose to the level of a black-box warning.” No cases were seen in the Vertex clinical trial”, she said.